November 30th, 2023 § Comments Off on Another Pause to Reflect § permalink
It’s hard to believe that my last post was in 2015, almost 5 years before the COVID-19 pandemic hit in force. I started this blog to answer questions that my patients were asking me, and I answered quite a lot here. When it began, it was 2010, a scant 6 years after the debut of Facebook, 4 years after Twitter, and only 3 years after the first iPhone. Much has happened since then.
In my last post, I wrote that you could follow me on Twitter. That was before Twitter sold itself, renamed itself X, and removed nearly all content moderation. I no longer go there.
I’ve kept the engine in this blog running smoothly so that you can search for topics, explore the archives, and use the word cloud. The information is still good and timely.
We’re entering a golden age of male reproductive medicine with new diagnostic tools and the promise of medicines specifically designed to treat male infertility. From time to time I’ll post the big advances here. But for now, enjoy and explore the site.
June 24th, 2013 § § permalink
An article in press in Fertility and Sterility is getting a lot of media attention. The study connected men seeking infertility care to a cancer registry in the State where the clinic was located. The researchers found that men with infertility had almost twice the chance of getting cancer and almost three times the chance if the man had no sperm in his ejaculate.
The authors of the study have a few theories about why cancer and male infertility may be connected. Cells need to divide just right to make sperm in the testes, and problems with division could lead to both problems with making sperm and the kind of bad division that makes cancer. It could also be that toxic substances in the environment may lead to both infertility and cancer.
Whatever the reason, we’re beginning to understand that problems with male fertility are just a tip of a much bigger iceberg that involves health in general. It’s more than just about the testicles.
August 16th, 2011 § § permalink
By Eve Feinberg, M.D.
Fertility Myths
Myth #1: Missionary position is best.
As long as intercourse is vaginal (and yes, strangely, I have had a few couples who had not grasped this detail prior to their first consultation), position does not matter. Sperm are incredible swimmers and studies have shown that within minutes of intercourse the sperm can be found within the fallopian tubes and will get to where they need to be expeditiously.
Myth #2: You should lie still for 30 minutes after intercourse with your legs in the air.
Sperm are incredible swimmers (see #1). It will not decrease your likelihood of conceiving if you use the bathroom or walk around within minutes of intercourse.
Myth # 3: I got pregnant and had an abortion in high school, so I am highly fertile.
Most high school students are highly fertile, but fertility declines with advancing age. Girls are born with a set number of eggs and over the course of a woman’s reproductive life, the number of eggs declines dramatically. There are several critical periods where the decline is more steep and after the age of 45, there is such little benefit to IVF using your own eggs, that most clinics will not perform IVF on a 45 year old woman attempting conception with her own eggs. On a good note, having had an abortion does not make you infertile.
Myth #4: I am a “young” 40.
Aging occurs at a variable rate when it comes to gray hair and wrinkles. Ovarian aging, unfortunately, is quite predictable. Your ovaries will never act younger than your chronological age. They may respond more robustly than expected and may give you a higher yield of eggs, but the quality of those eggs is linked to a woman’s age. And sadly, egg quality and quantity decrease markedly with advancing age.
Myth #5: If you relax, you will get pregnant.
There are very few cases where the sole cause of infertility or IVF success is stress. This is a common perception and often a hurtful thing to say to an infertile couple. Infertility is a medical condition with identifiable, organic causes in the majority of cases. There has not yet been a well designed study that shows the positive impact of stress reduction on conception success.
I hope you’ve enjoyed Fertility Myths (and my VERY FIRST) blog entry ever. I am excited to be on the blogosphere and welcome your comments or suggestions for new topics.
April 4th, 2011 § § permalink
Your semen analysis results came back, and it says that you have a lot of white blood cells. What does it mean?
White blood cells are the body’s soldiers to fight invaders like bacteria and viruses, and their presence in semen might signal an infection. White cells also produce superoxide radicals, bullets that riddle sperm and its precious DNA cargo.
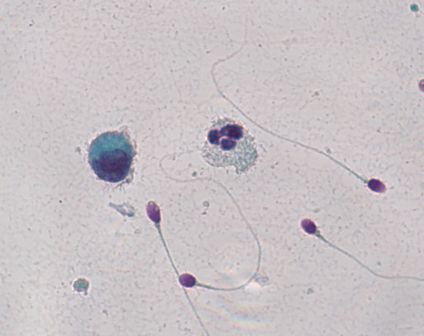
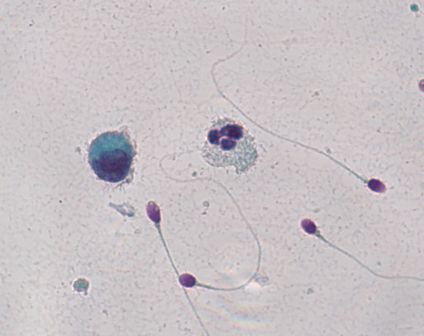
Here’s the problem: you might not have white blood cells at all. If you put semen under the microscope, white blood cells look exactly like immature sperm cells that aren’t a problem at all. A technician needs to stain the cells to see which cells are the bad actors. In the picture, an innocuous cell is on the left, and to its right lies an angry white blood cell. It’s easy to tell the difference because they’ve been stained. But without the coloration from staining, it would be impossible to say which was which.
Unfortunately, not all labs routinely stain semen if large round cells cells are present in high amounts. Specialized semen analysis labs typically will, but general laboratories performing many different kinds of tests may not.
If your test, with staining, confirms that you do have an unhealthy amount of white blood cells in the semen, what can you do? Culturing semen in the lab doesn’t usually reveal the bacterial invaders. The prostate turns out to be remarkably good at hiding infection, making it a difficult job to find the bug causing the problem. Doctors often try a course of broad spectrum antibiotics to attack anything that may be lurking. Another strategy is to use an antioxidant like coenzyme Q10 to protect the sperm from the white blood cell’s superoxide radicals.
But first you have to know if you’re dealing with white blood cells.
March 21st, 2011 § Comments Off on Radiation and Sperm § permalink
The horrific earthquake and tsunami in northern Japan remind us that no matter how powerful we become or careful we are, nature asserts itself in ways that we can’t imagine. The nuclear engineers and technicians working to contain the radiation leaking from the damaged power plant in Fukushima are nothing short of heroic. Radiation can cause all sorts of ills, from acute sickness to cancer and infertility.
In the testis, developing sperm cells are exquisitely sensitive to radiation. Kyodo News reported that after an explosion at the Fukushima No. 2 reactor on March 15, radiation levels measured as high as 8,217 micro sievert or 0.8217 rem per hour. (Micro sievert and rem are units of radiation dosage.)
Does that amount of radiation harm developing sperm cells? I asked Marvin Meistrich, Ph.D., Professor of Experimental Radiation Oncology and the Florence M. Thomas Professor of Cancer Research at the University of Texas M. D. Anderson Cancer Center, a world’s expert in radiation and sperm. Dr. Meistrich explained that sustained exposure to 20 rem of radiation over 4 weeks caused sperm counts to drop to 1/10th of their original amount. At doses of 40-80 rem, sperm counts fell to about 1/100th of the starting number, and in some cases were wiped out entirely. At 200 rem, that drop to zero sperm became permanent. For one-time doses, Dr. Meistrich explained that 15-20 rem caused a short-term fall in sperm count, and 400 rem or more resulted in permanent loss of sperm.
We know that radiation changes DNA, the sperm’s precious genetic cargo. What we don’t know is what dose causes a harmful DNA change that damages a developing embryo or causes disease later in life.
The radiation leakage in Fukushima seems to be in the range at which damage to sperm occurs. I can only hope that the workers at Fukushima and the people near the plants are aware of the dangers and take action to protect themselves.