February 21st, 2012 § § permalink
SpermCheck has arrived and is filling the shelves of your neighborhood drug store as I write. What is it? It’s an over-the-counter FDA approved home male fertility test. What does it do? It tells you whether you have more than 20 million sperm per milliliter of semen.
That’s a good thing, right? Generally, yes. It’s good to know whether you have a reasonable amount of sperm, which SpermCheck says is 20 million per milliliter. The problem is in the yes-or-no nature of the test and in picking the number 20 million. As I described in this post, you can get a woman pregnant with sperm counts less than 20 million per milliliter and have problems with more than that amount. The numbers of swimmers don’t tell the whole story.
So, will SpermCheck help you? For most men, probably. Having a positive or negative result will point them in the right direction. But for the handful of guys that get the OK from the test when they have a problem or for those that get the thumbs-down from the test that are fertile, it’s not telling the whole story. According to the manufacturer, the guys that are getting it wrong is about one in twenty. If you’re OK with that, great–if not, you may want to see a doctor.
April 16th, 2011 § § permalink
After last week’s post about pus in semen, I thought that it might be helpful to describe another important sperm test, one that shows whether or not they’re alive.
Good sperm are alive. Not only do they swim, they live and breathe just as all living cells do. Some are dead, meaning that the ship is no longer sailing, and its motor and crew are gone.
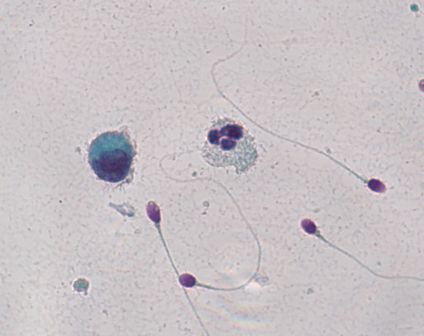
One way of figuring out whether or not sperm are alive is to dip them in colored dye. A dead sperm can’t push the dye out of its body, but a live sperm can. In the picture, the sperm are stained with a pink dye called Eosin. The dead sperm are the ones that become pink, and the live sperm are the ones that push the dye outside and stay clear (a light bluish green in the photograph.)

The result of the test is typically described in the percentage of sperm that are alive, and of course, the more living sperm the better. But even when all of the sperm are dead, a condition called “necrospermia”, couples can still conceive using in-vitro fertilization with intra-cytoplasmic sperm injection.
That doctors can successfully use dead sperm with in-vitro fertilization illustrates a conundrum in reproductive medicine today. The ultimate barrier to fertilization is no longer the entire sperm’s health, but the quality of its DNA cargo. Unfortunately, we don’t yet have a way of knowing the condition of a single sperm’s DNA before inserting that sperm into an egg.
So if a man’s sperm don’t wiggle, the first thing to know is whether they’re alive and sluggish or whether they’re dead. A vital stain makes that distinction. But if they’re dead, a man shouldn’t despair. Dead sperm can still be used in intra-cytoplasmic sperm injection as long as their DNA is good. Unfortunately, the only way to know that right now is to inject the sperm and to see what happens.
April 4th, 2011 § § permalink
Your semen analysis results came back, and it says that you have a lot of white blood cells. What does it mean?
White blood cells are the body’s soldiers to fight invaders like bacteria and viruses, and their presence in semen might signal an infection. White cells also produce superoxide radicals, bullets that riddle sperm and its precious DNA cargo.
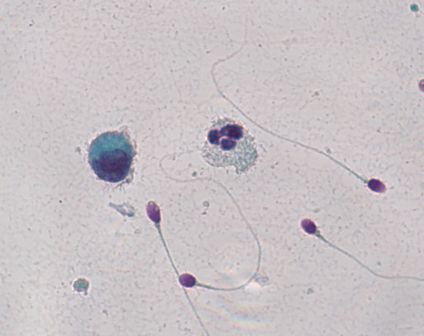
Here’s the problem: you might not have white blood cells at all. If you put semen under the microscope, white blood cells look exactly like immature sperm cells that aren’t a problem at all. A technician needs to stain the cells to see which cells are the bad actors. In the picture, an innocuous cell is on the left, and to its right lies an angry white blood cell. It’s easy to tell the difference because they’ve been stained. But without the coloration from staining, it would be impossible to say which was which.
Unfortunately, not all labs routinely stain semen if large round cells cells are present in high amounts. Specialized semen analysis labs typically will, but general laboratories performing many different kinds of tests may not.
If your test, with staining, confirms that you do have an unhealthy amount of white blood cells in the semen, what can you do? Culturing semen in the lab doesn’t usually reveal the bacterial invaders. The prostate turns out to be remarkably good at hiding infection, making it a difficult job to find the bug causing the problem. Doctors often try a course of broad spectrum antibiotics to attack anything that may be lurking. Another strategy is to use an antioxidant like coenzyme Q10 to protect the sperm from the white blood cell’s superoxide radicals.
But first you have to know if you’re dealing with white blood cells.
June 9th, 2010 § § permalink
A first test of male fertility is the semen analysis. You do your thing, and a technician counts the sperm, sees how they’re moving, what they look like and whether they’re alive. For decades, the World Health Organization has published criteria for these numbers to alert a man that he might have a problem when it comes to impregnating a woman. Until recently, the numbers were a consensus of expert opinion, but in the latest edition, the WHO criteria changed substantially.
What the WHO is currently doing is to dispense with expert opinion, and just lay the numbers out for all to see. Table II from the paper shows the numbers for men from couples who conceived within a year. Take sperm concentration, for example. For centile 5, the sperm concentration is 15 million per ml. That means that only 5% of couples where the man had 15 million/ml sperm or less conceived within a year. For centile 50, the concentration was 73 million/ml, meaning that 50% of couples conceived within a year when the sperm concentration was up to that number. You get the idea.
The problem is that people like cutoffs, and in the latest edition, the WHO chose centile 5 as the line in the sand. It’s a good number for thinking that below it, couple infertility likely involves the male. But keep in mind that at centile 10, only 10% of couples conceived within a year. In other words, having sperm numbers above the centile 5 cutoff doesn’t guarantee that the sperm are trouble free.
Frankly, I think the WHO numbers are most useful to get a ballpark idea of how fertility may be related to what’s inside the semen. I prefer the approach David Guzick and colleagues took, where they applied a statistical method called Classification and Regression Tree (CART) analysis to sperm, which gives two cutoffs in a “green light, yellow light, red light” fashion. For example, CART analysis came up with 13.5 million/ml and 48 million/ml for sperm concentration. At 13.5 million/ml sperm or less, the “red light,” couple infertility likely involves the male. At 48 million/ml or more, your sperm probably are “green light” good to go. Between 13.5 million/ml and 48 million/ml, the “yellow light,” sperm may or may not be the problem. You can find the Guzick CART cutoffs here.
A lot of people, including doctors and fertility specialists, are confused about the new WHO cutoffs. Expect a little consternation about them for a bit.
WHO Table II Distribution of values, lower reference limits and their 95% CI for semen parameters from fertile men whose partners had a time-to-pregnancy of 12 months or less
|
N |
Centiles
|
|
|
|
|
|
|
|
|
|
|
|
2.5 |
(95% CI) |
5 |
(95% CI) |
10 |
25 |
50 |
75 |
90 |
95 |
97.5 |
|
| Semen volume (ml) |
1941 |
1.2 |
(1.0–1.3) |
1.5 |
(1.4–1.7) |
2 |
2.7 |
3.7 |
4.8 |
6 |
6.8 |
7.6 |
| Sperm concentration (106/ml) |
1859 |
9 |
(8–11) |
15 |
(12–16) |
22 |
41 |
73 |
116 |
169 |
213 |
259 |
| Total number (106/Ejaculate) |
1859 |
23 |
(18–29) |
39 |
(33–46) |
69 |
142 |
255 |
422 |
647 |
802 |
928 |
| Total motility (PR + NP, %)* |
1781 |
34 |
(33–37) |
40 |
(38–42) |
45 |
53 |
61 |
69 |
75 |
78 |
81 |
| Progressive motility (PR, %)* |
1780 |
28 |
(25–29) |
32 |
(31–34) |
39 |
47 |
55 |
62 |
69 |
72 |
75 |
| Normal forms (%) |
1851 |
3 |
(2.0–3.0) |
4 |
(3.0–4.0) |
5.5 |
9 |
15 |
24.5 |
36 |
44 |
48 |
| Vitality (%) |
428 |
53 |
(48–56) |
58 |
(55–63) |
64 |
72 |
79 |
84 |
88 |
91 |
92 |
|
*PR, progressive motility (WHO, 1999 grades a + b); NP, non-progressive motility (WHO, 1999 grade c).
May 27th, 2010 § § permalink
If you’re trying to get pregnant, something useful to know is how often to have sex. Sperm counts peak at two to three days after ejaculation, meaning, after you have sex (or masturbate,) the swimmers will be most abundant two to three days later. Sperm live for about 48 hours in the female reproductive tract, so the optimum timing is sex every other day.
However, don’t freak out if you have an especially romantic weekend with a little extra frequent activity, or get caught up and miss a few days. Stressing out about sex is counter productive, as stress itself can result in poorer sperm quality.
I’m often asked when during the month (or cycle) a couple should try to conceive. Studies show that conception usually happens up to six days before, and ending on, ovulation. The big problem is that all tests for ovulation show the event after it happens. So a good plan is start having sex every other day after menstruation ends, and keep going until the next menstruation.
So, soldier on. Have sex every other day. Doctors orders.