January 23rd, 2011 § § permalink
Has it really been over three months since my last post? Between becoming one of the next Co-Editors in Chief of Fertility and Sterility, preparing for a review of our urology training program and finishing my latest book (Thank You, Chapter Authors!) I guess that I’ve let my blogging slip a bit. Fortunately, thanks to my Italian co-faculty’s discovery of the Saeco Vienna Plus espresso maker at Costco, I’m back at the keyboard.
I turned off the two-week limit for comments, and so far, that’s been a good idea. People are commenting on older posts (like How Clomid Works in Men) with good questions and thoughtful points. For new commenters, please read the FAQ. I can’t answer questions about specific patients. Those are best left to a live visit with a doctor with an interest in male reproductive medicine. One great resource is the American Society for Reproductive Medicine’s Society for Male Reproduction and Urology page and the ASRM’s find a doctor search page, (just click on the “Society for Male Reproduction and Urology (SMRU)” button in the “Find Member by Affiliated Society:” section.) Another excellent way to find a specialist who treats men with reproductive issues is to use the American Urological Association’s Society for the Study of Male Reproduction’s search engine.
This blog post was inspired by several patients who asked after I explained surgical sperm retrieval, if there was somewhere they could go for more information. I realized that I hadn’t written about such a common issue.
Just as a carpenter has many ways to make a cabinet, a surgeon can tackle a problem in a number of ways. And just as two cabinets may differ, different surgical problems demand different approaches. Such is the case in retrieving sperm from the testis.
Most of the time, taking sperm directly from the testis is necessary when a man has azoospermia, where no sperm is found in the ejaculate. Azoospermia takes two basic forms, obstructive and non-obstructive. As the name implies, obstructive azoospermia is due to a blockage in the tubes and structures that convey sperm from the testis to the outside world. In the best case, a surgeon can fix the errant anatomy, allowing a couple to conceive children without further ado. But because the tubes are so tiny, sometimes the tubes can’t be reconnected with surgery, and the alternative is to take sperm from the testis for it to be used in in-vitro fertilization.
The other form of azoospermia, non-obstructive, arises when the factory making sperm in the testis isn’t working quite right. Sometimes, the cells starting sperm are missing entirely, a condition known as “Sertoli cell only syndrome”. Occasionally, sperm may be rolling along their assembly line, a process that takes two to three months to complete, and stop mid-production. When that happens, it’s called “maturation arrest“. But frequently, sperm can be found in small amounts in the testis and can be retrieved using surgery.
 Because it isn’t mature, sperm from the testis can only be used with in-vitro fertilization and intra-cytoplasmic sperm injection.
Because it isn’t mature, sperm from the testis can only be used with in-vitro fertilization and intra-cytoplasmic sperm injection.
How can a surgeon remove sperm? He or she can take it from the testis itself, or the epididymis, the tiny coiled tube lying on the back of the testis where sperm mature. The surgeon can insert a needle into the testis or epididymis, he or she may make one or several small incisions into the testis or use microsurgery to retrieve sperm from either the testis or epididymis. In the case of obstructive azoospermia, it doesn’t seem to matter which technique is used. There’s plenty of sperm wherever it’s sought, and any method will do to retrieve it. When a man has obstructive azoospermia, I usually recommend taking a small piece from the testis, as the sperm may be frozen and is good for a number of in-vitro fertilization cycles so that the man doesn’t need to go through a procedure for every cycle, and can be there for his wife during her procedures.
 We’ve found that frozen sperm is just as good as fresh. in fact, the chances for fertilization are the same for fresh and frozen sperm, and the chance for pregnancy may even be a little better for frozen sperm than for fresh.
We’ve found that frozen sperm is just as good as fresh. in fact, the chances for fertilization are the same for fresh and frozen sperm, and the chance for pregnancy may even be a little better for frozen sperm than for fresh.
 Frozen sperm should literally last forever. It’s in liquid nitrogen, which is so cold that the building blocks making sperm don’t decay. Freezing sperm gives a couple time to plan when in-vitro fertilization is done.
Frozen sperm should literally last forever. It’s in liquid nitrogen, which is so cold that the building blocks making sperm don’t decay. Freezing sperm gives a couple time to plan when in-vitro fertilization is done.
When he has non-obstructive azoospermia, a man’s options are more limited. A surgeon can use the operating microscope to comb through the testis looking for areas that may contain sperm, a procedure known as “microsurgical testis sperm extraction“. Other techniques include making several small incisions in the testis or piercing the testis with a needle in a dozen or so different spots. When a man has non-obstructive azoospermia, I usually recommend microsurgical testis sperm extraction. More areas of the testis can be examined, and I can see the places that most likely contain sperm.
We’ve observed that prescribing a man with non-obstructive azoospermia clomiphene citrate for a few months before surgical retrieval seems to increase the chance to retrieve sperm. In many men, sperm appears in the ejaculate and surgery isn’t needed. If a couple has a few months, taking clomiphene before surgical sperm retrieval might be a good idea.
In short, a surgeon has many ways to retrieve sperm when necessary. The choice depends on the preference of the surgeon and the couple, and what’s going on inside the testis. I’ve listed the surgical techniques available, and my typical recommendations.
June 16th, 2010 § § permalink
The testes must be kept cool for the proper production of sperm. One way the human body achieves this is to house them outside the body. Another is to have a network of veins surrounding the artery pumping blood into the testis: the veins take the heat away in a “counter-current” heat exchange similar to a radiator. (The human body is an amazing piece of engineering.)
Arteries don’t need to worry about moving blood; there’s a huge amount of pressure coming from the heart to help with that. But once the blood goes through the capillaries and into the veins, getting back to the heart isn’t easy. Veins have little valves to help hold the blood while it pulses its way back. If those little valves start to separate, the vein expands, causing the condition known as a “varicose vein.” Varicose veins can happen in many places in the body, often visibly in the skin of the legs, but, believe it or not, also in the scrotum. And if varicose veins develop in the scrotum, they can disturb the counter-current heat exchange. The testes then get hot, posing a problem for developing sperm cells.
Varicose veins in the scrotum are called a “varicocele,” and there are three kinds. A grade I varicocele can’t be felt or seen without equipment like ultrasound. Almost all experts now consider grade I varicoceles to be unimportant. Varicoceles that can be felt (grade II) or visible by the naked eye (grade III) are the ones that may cause problems with sperm production. Some men have such high sperm production that their varicoceles don’t significantly alter their chance of making women pregnant. But many men’s testes are affected by grade II or III varicoceles.
Inside of a man, the left vein draining the testis back towards the heart is longer than the right. As a result, varicoceles are most often found in the left scrotum. Sometimes, they’re on both sides, and infrequently, they’re on the right side alone. A right sided varicocele that suddenly appears in adult life is worrisome, as it may be a sign of kidney cancer.
What can be done about a varicocele that may be throwing a wrench into the sperm factory? A urologist can tie or clip the veins in a procedure called “varicocelectomy,” or an interventional radiologist can inject material into the veins to block the flow of blood.
April 28th, 2010 § § permalink
With the suspension of Cincinnati Reds pitcher Edinson Volquez for performance enhancing drug use and a swirl of rumors that the agent involved was clomiphene (also known as Clomid,) I thought it timely to write about how clomiphene works and how it’s used. From what I read on the internets, there is an enormous amount of misinformation floating around out there.
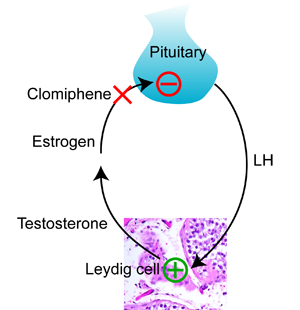
To understand how clomiphene works, you need to know how the pituitary controls the making of testosterone in the testis. Testosterone is made by Leydig cells in the testis, which I explained in my last post. The pituitary releases a hormone called luteinizing hormone (“LH”) that stimulates the Leydig cells to make testosterone. Testosterone is converted to the female hormone estrogen, (which I also explained in my last post,) and estrogen tells the pituitary to stop making more LH. This kind of negative feedback system is common when it comes to how hormones work. It’s just like a thermostat and heater. As the room gets warmer, the thermostat sends less electricity to the heater. When the room gets colder, the thermostat sends more electricity to the heater.
Clomiphene works by blocking estrogen at the pituitary. The pituitary sees less estrogen, and makes more LH. More LH means that the Leydig cells in the testis make more testosterone.
As I explained in my last post, giving testosterone to a man does just the opposite. The pituitary thinks that the testis is making plenty of testosterone, and LH falls. As a result, the testis stops making testosterone, and the usually high levels of testosterone in the testis fall to the lower level in the blood.
So clomiphene is a way to increase testosterone in the blood and the testis at the same time. It preserves testis size and function while increasing blood testosterone.
Unfortunately, clomiphene is not FDA approved for use in the male. Like most of the medications that we use to treat male fertility, the pharmaceutical company that originally sought approval by the FDA did it for women. Clomiphene is now generic, and it’s unlikely that anyone will pony up the hundreds of millions of dollars necessary to get it approved for the male. That’s the bad news. The good news is that it means that this medication is fairly inexpensive, cheaper than most forms of prescription testosterone. Can a doctor prescribe clomiphene for a man? Yes. It’s “off label”, meaning that it’s not FDA approved for use in men.
As a medication, clomiphene is usually well tolerated by men. In my experience, most patients don’t feel anything as their testosterone rises. Those that do feel an increase in energy, sex drive, and muscle mass, especially if they work out. Very rarely I’ve had patients report that they feel too aggressive, or too angry. Very very rarely (twice in the last 20 years) I’ve had patients report visual changes. That’s worrisome, as the pituitary is near the optic nerve in the brain, and visual changes suggests that the pituitary may be changing in size. Because the skull is a closed space, it’s alarming if anything in the brain changes in size. In the last twenty years, I’ve also had two patients who had breast enlargement (called “gynecomastia”) while using clomiphene. Needless to say, for any of these problematic side effects, the clomiphene is discontinued.
So that’s the story with clomiphene. It can be used in the male, either for fertility or low testosterone levels. It’s an off label prescription drug. It works, and is usually well tolerated by men who take it.
April 28th, 2010 § § permalink
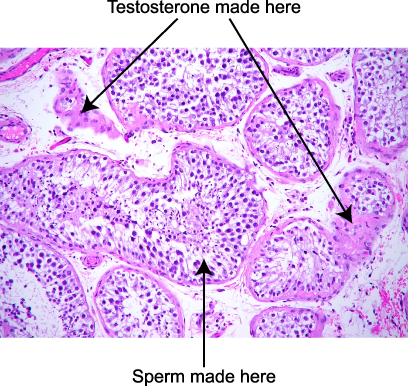
When you think of what makes up the inside of the testes, think spaghetti. Imagine a bunch of spaghetti noodles squished together. Inside of the noodles are the developing sperm cells. Between the noodles are cells called “Leydig cells” whose job it is to make the male hormone testosterone. They start with cholesterol, and churn out testosterone.
Not only is testosterone critical to the factory inside the spaghetti that makes sperm, it is important for many parts of the male body to work well. Adequate testosterone is needed for bone and muscle strength, and men with low testosterone may experience low sex drive, problems with mental focus and depression.
The relationship between testosterone and how the penis works is less clear. Men with low testosterone can get erections, but of course sex drive can be a problem. And if a man’s testosterone is low, correcting it may improve the performance of drugs like Viagra, Levitra and Cialis.
Total testosterone doesn’t tell you the whole story. Testosterone circulates in the blood in two forms. Testosterone that is either free or loosely bound to blood protein is called “bioavailable”, and as the name implies, is available for the cells to work. Testosterone that is bound to sex hormone binding globulin (“SHBG”, but also called androgen binding protein,) is blocked from acting in cells. Although many labs offer to measure free testosterone, often the most reliable way to measure bioavailable testosterone is to have the blood tested for albumin, sex hormone binding globulin and testosterone, and then to use a calculator for bioavailable testosterone. One is available on the International Society for the Study of the Aging Male’s web site, and another for iPhones and iPod touches can be found in the iTunes store. A man may have adequate total testosterone, but still suffer from the ravages of low testosterone levels if his bioavailable testosterone is low.
Testosterone levels rise and fall during the day, with a peak in the early morning, and the lowest point in the late afternoon. That’s why many a man’s sex drive is highest in the morning, and it’s time for a nap in the afternoon.
Testosterone is converted to dihydrotestosterone, which makes the hair fall out of your hair follicles if your family tree has male pattern baldness. Dihydrotestosterone also enlarges the prostate. Drugs like finasteride (Propecia and Proscar) and dutasteride (Avodart) block the conversion of testosterone to dihydrotestosterone.
All men have a little estrogen, the female hormone. An enzyme called “aromatase” converts testosterone to estrogen. If the estrogen level is too high, it may interfere with the working of testosterone.
One last important point about the making of testosterone: levels in the testis are twenty times greater than in the blood. So if a man is given testosterone, his blood levels may increase, but the pituitary tells the testis, “hey, there’s enough testosterone around, so stop making it.” As a result, testosterone levels in the testis fall, sperm stop being made, and the testes shrink. That’s why many body builders who take testosterone and other similar chemicals experience shrinking testes. Testosterone can be great for men with low levels later in life, but for men who want to have children, it can really work against sperm production.
![]() Because it isn’t mature, sperm from the testis can only be used with in-vitro fertilization and intra-cytoplasmic sperm injection.
Because it isn’t mature, sperm from the testis can only be used with in-vitro fertilization and intra-cytoplasmic sperm injection.![]() We’ve found that frozen sperm is just as good as fresh. in fact, the chances for fertilization are the same for fresh and frozen sperm, and the chance for pregnancy may even be a little better for frozen sperm than for fresh.
We’ve found that frozen sperm is just as good as fresh. in fact, the chances for fertilization are the same for fresh and frozen sperm, and the chance for pregnancy may even be a little better for frozen sperm than for fresh.![]() Frozen sperm should literally last forever. It’s in liquid nitrogen, which is so cold that the building blocks making sperm don’t decay. Freezing sperm gives a couple time to plan when in-vitro fertilization is done.
Frozen sperm should literally last forever. It’s in liquid nitrogen, which is so cold that the building blocks making sperm don’t decay. Freezing sperm gives a couple time to plan when in-vitro fertilization is done.